The ongoing quest to unravel the complexities of treating mood disorders has been marked by reliance on selective serotonin reuptake inhibitors (SSRIs). These drugs have become widely prescribed for anxiety and depression, yet their mechanisms and long-term effects remain subjects of debate. Recent research led by Vibeke Dam from Copenhagen University has further explored this landscape, examining how SSRIs impact both cognitive abilities and mood in individuals suffering from moderate to severe depression.
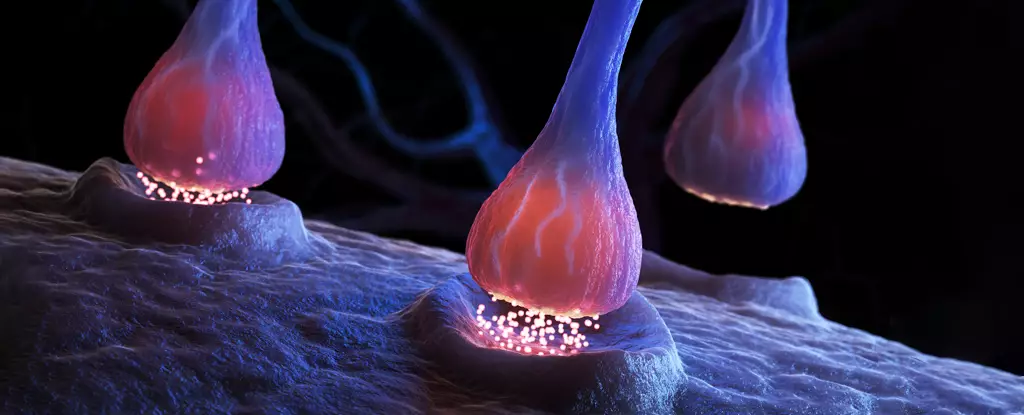
SSRIs work by increasing the levels of serotonin—a neurotransmitter associated with mood regulation—in the brain. Despite their prevalence in treatment plans, many practitioners and patients question the robustness of SSRIs’ therapeutic effects. Doubts arise from a lack of concrete evidence demonstrating their long-term efficacy and a thorough understanding of how they modify brain function over time. The ongoing scrutiny is crucial in light of emerging studies that suggest SSRIs may not outperform placebos for a considerable percentage of patients, challenging the traditional view of serotonin as a central player in mood disorders.
Dam and her team meticulously examined the effects of the SSRI escitalopram on 90 patients through a series of brain scans and cognitive assessments. This rigorous study employed both imaging techniques and standardized tests, now focusing on patients before and post-eight-week treatment. The findings revealed significant changes, particularly in receptor levels, indicating that SSRIs could reduce the availability of serotonin receptors, which are critical for neurotransmission and cognitive processing.
Interestingly, while there was nearly a 10 percent decrease in the serotonin receptors post-treatment, cognitive assessments indicated notable improvements in verbal memory among the patients. Specifically, those who exhibited minimal changes in the 5-HT4 receptor showed the best enhancements in their ability to recall words. This correlation suggests that while receptor binding may diminish, the functional capacity of remaining receptors could improve through enhanced serotonergic activity.
Perhaps the most puzzling aspect of this study was the disconnection between mood improvements and changes in the 5-HT4 receptors. While some patients demonstrated cognitive gains, the anticipated mood elevation did not directly parallel the alterations in receptor status. This discrepancy raises critical questions about the established understanding of how SSRIs exert their effects. It appears that cognitive enhancement may not rely solely on the reduction of receptor levels but could involve a complex interplay between ongoing serotonergic activity and receptor efficiency.
The implications of these findings are twofold. First, they underscore the need for more precise targeting in antidepressant treatments, particularly focusing on the less understood areas of serotonin function and receptor activity. Second, it suggests that future pharmaceutical strategies might benefit from a dual approach that combines cognitive enhancement with mood improvement, particularly in patients for whom traditional antidepressant treatments have not yielded satisfactory results.
Despite the promising results, the study faced ethical limitations, notably the absence of a placebo group. This aspect may lead to questions regarding the reliability of the findings, as the absence of a control group complicates the ability to attribute cognitive improvements conclusively to the SSRIs themselves. Moreover, the long-held assumption regarding serotonin’s role in depression continues to be scrutinized, leaving room for doubt about SSRIs’ overall efficacy.
As we navigate this intricate terrain, it is crucial for both clinicians and researchers to carry out further investigations that can clarify the mechanisms through which SSRIs operate, not only for cognitive enhancement but also for addressing mood symptoms. The potential exists not merely for developing new medications but for refining existing treatment protocols to incorporate holistic patient care in managing mood disorders.
While SSRIs remain a cornerstone in treating depression and anxiety, the findings highlighted by Dam and her colleagues prompt a reevaluation of how these medications are perceived and utilized. The path forward must entail a commitment to disentangling the multifaceted relationships between cognitive function, mood regulation, and serotonin levels, ultimately paving the way for more effective treatments rooted in scientific understanding rather than assumption.

Leave a Reply