As we progress through life, our bodies undergo a multitude of changes, some beneficial and some detrimental. Among the most concerning changes is the age-related evolution of cancer risk, which presents a perplexing duality. Throughout our 60s and 70s, the accumulation of genetic mutations significantly elevates the likelihood of developing cancer. However, intriguingly, this risk begins to decline after the age of approximately 80. Recent research offers compelling insights into this phenomenon, providing potential avenues for better understanding cancer development and treatment in older individuals.
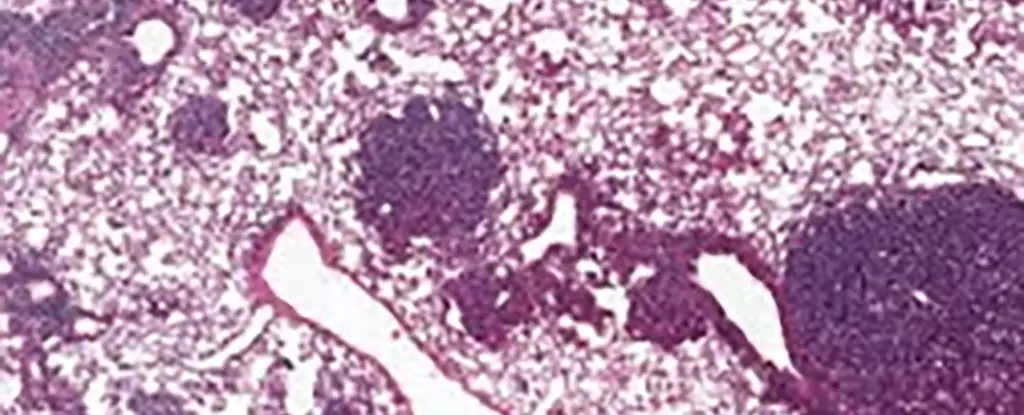
A recent collaborative study delved into the mechanisms driving lung cancer by investigating alveolar type 2 (AT2) stem cells in mice. These specialized cells play an essential role in the lung’s regenerative processes as well as in the onset of lung cancer. The researchers discovered elevated levels of a specific protein, NUPR1, in older mice, which appears to interfere with the normal regenerative capacity of these cells.
NUPR1 has been linked to cell responses related to iron metabolism. In aging cells, even though there is an abundance of iron present, their behavior mimics that of cells that are iron-deficient. This contradiction arises from molecular changes that occur as we age, leading these cells to lose their ability to proliferate effectively. Cancer biologist Xueqian Zhuang from Memorial Sloan Kettering Cancer Center suggests that the aging process diminishes stem cells’ renewal capabilities, providing fewer opportunities for uncontrolled cell proliferation — a hallmark of cancer.
The study did not limit itself to mouse models but extended its inquiry into human cells. Similar findings emerged: increased levels of NUPR1 negatively correlated with the amount of iron cells could utilize, hampering their growth. Encouragingly, interventions such as artificially reducing NUPR1 levels or enhancing iron supply resulted in boosted cell growth, highlighting a potential target for therapeutic exploration.
This discovery unveils promising prospects for future cancer treatments, particularly concerning iron metabolism. For instance, these insights could lead to innovative approaches for restoring lung function in individuals facing prolonged recovery from illnesses like COVID-19. Furthermore, they open the door to understanding how altered iron states in older cells influence resistance to contemporary cancer therapies, particularly those relying on ferroptosis, a form of cell death linked to iron regulation.
This cutting-edge research brings vital implications for cancer prevention strategies. Tuomas Tammela, another key researcher from MSK, emphasizes that younger individuals are more affected by carcinogenic activities, such as smoking and excessive sun exposure. Preventive measures aimed at reducing these risks could yield significant benefits — potentially mitigating the cumulative genetic damage that heightens cancer risk in older age.
Additionally, the nuanced understanding of how aging influences cancer biology could guide personalized treatment methodologies. As individual responses to treatment vary significantly based on age, cancer type, and existing health conditions, integrating these factors into treatment plans could enhance efficacy. Recognizing the fluid interplay between aging and cancer progression remains a critical focus for ongoing research.
Despite the strides made in understanding the relationship between aging and cancer risk, there remains a vast expanse of knowledge yet to be uncovered. Researchers continue to grapple with the complex biology that governs how age alters not just cancer’s incidence but also its progression and treatment response. Continued investigation into NUPR1’s role in stem cell function and cancer development will be essential for advancing therapeutic options.
The dual nature of aging as it relates to cancer risk underscores the significance of both prevention and treatment tailored to the individual. By probing deeper into the mechanisms of aging, scientists hold the key to unlocking more effective strategies for combating cancer across different life stages. The journey toward comprehensive cancer care is ongoing, but new findings like those surrounding NUPR1 pave the way for a more sophisticated understanding of how we confront this formidable disease.

Leave a Reply