The recent discovery by researchers of a process in fruit flies that connects inflammation with impaired motor function has provided new insights into potential treatment options for the persistent muscle fatigue experienced by many individuals following infections. Long COVID, with its array of symptoms, includes an intolerance to exertion that can be particularly debilitating. According to developmental biologist Aaron Johnson from Washington University, this reduced energy levels in skeletal muscle can significantly decrease the capacity to move and function normally.
With each new infection of the SARS-CoV-2 virus, the risk of developing long COVID increases. A significant portion of adult Americans has now experienced the lingering malaise and physical symptoms associated with this condition, including muscle fatigue. This symptom is not unique to long COVID but is also present in other post-viral conditions and neurodegenerative diseases like Alzheimer’s and Parkinson’s, all of which involve inflammation of the central nervous system.
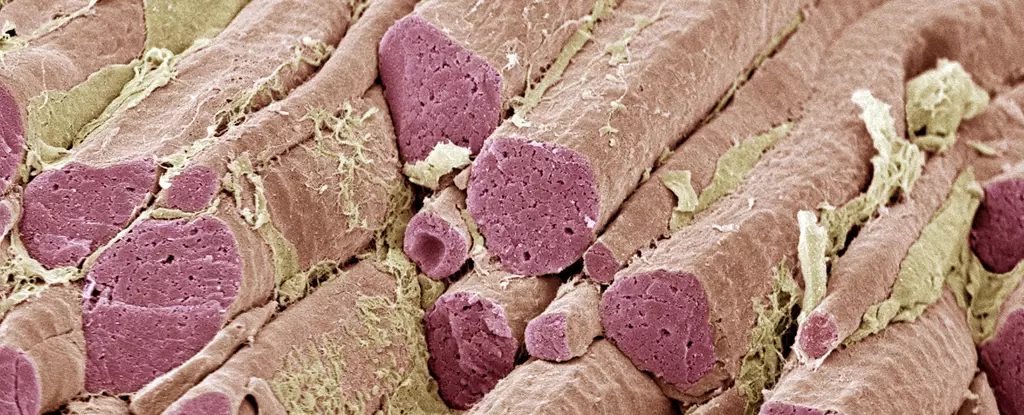
Washington University researchers, led by Shuo Yang, utilized animal models to investigate how inflamed neurons can lead to dysfunctional muscles. They discovered a signaling pathway between brain cells and muscles in flies and mice that ultimately results in a loss of muscle function. This effect was observed not only with COVID-associated proteins but also with proteins related to bacterial infections and Alzheimer’s disease. Interestingly, the reduced muscle performance can persist even after the infection has been cleared, suggesting a chronic impact on muscle function.
In humans, inflammation triggers neurons to release the immune cytokine interleukin-6 (IL-6). The researchers found a similar protein in their animal models that traveled to the muscles via the bloodstream and activated the JAK-STAT cellular program. This activation led to a decrease in the energy produced by the mitochondria in muscle tissues. Johnson speculates that this damaging signaling process from the brain to muscles may have evolutionary roots in reallocating resources to the brain during disease fighting.
The researchers were able to reverse this pathway in flies using drugs, similar to previous studies in mice. IL-6 inhibitors, which have been effective in treating autoimmune diseases and some severe COVID-19 cases, could hold promise in addressing the chronic cytokine signaling that may underlie long COVID. The research suggests that the brain-muscle axis may be activated by respiratory infections, continuing to signal long after the initial infection has been resolved.
While some aspects of this process are still uncertain, such as how SARS-CoV-2 enters the central nervous system to provoke inflammation, this discovery represents a significant step toward understanding the physical impacts of brain inflammation on the body. By modulating the chemicals released by neurons, researchers may uncover new avenues for treating a variety of chronic conditions with similar inflammatory origins. The potential for alleviating the symptoms of long COVID and related disorders is an exciting prospect that warrants further investigation.

Leave a Reply