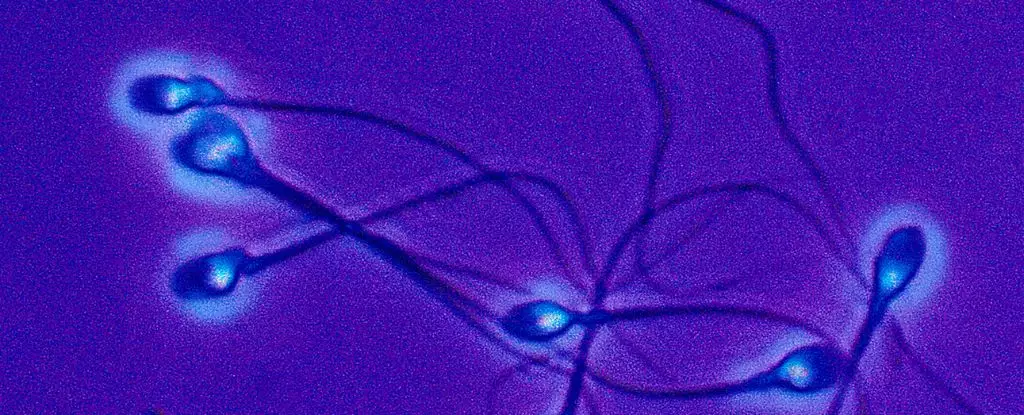
The human papillomavirus (HPV) has long been associated with cervical cancer in women, but recent research from Argentina has shed light on the impact of HPV on male fertility. The study found that high-risk strains of HPV are linked to a higher percentage of dead sperm in semen samples from adult males. These strains were also associated with a lower count of white blood cells and an increase in reactive oxygen species, which can damage sperm and alter DNA. This highlights a previously underexplored aspect of HPV’s impact on male reproductive health.
Despite the known risks of HPV to male health, the history of vaccination against the virus has been heavily gendered. When the HPV vaccine was first introduced in 2006, it was only approved for young female patients in the US. It took several years before the vaccine was also approved for young males, reflecting a persistent trend of overlooking HPV’s effects on men. Today, the World Health Organization recommends that both males and females receive the HPV vaccine, but boys are still considered secondary targets for vaccination.
Disparities in Vaccination Rates
The disparity in HPV vaccination rates between boys and girls is a major concern in global public health. In 2019, only 4 percent of boys globally had received the full course of the vaccine, compared to 15 percent of girls. In the US, vaccination rates among teen boys are slightly lower than for girls, at 61 percent versus 65 percent. These disparities may be fueled by misconceptions about the vaccine’s purpose, with many boys questioning why they should receive a vaccine primarily targeted at girls.
The Need for Inclusive Vaccination Programs
The recent research from Argentina underscores the importance of including boys in HPV vaccination programs. The study found that men infected with high-risk HPV strains showed significant changes in sperm quality, potentially impacting their reproductive health and the health of their offspring. As throat and penile cancers associated with HPV continue to rise, there is a growing consensus that universal vaccination against HPV is crucial to eradicating the virus and its health consequences.
The pervasive view of HPV as a “woman’s problem” has long obscured the virus’s impact on male fertility. By focusing primarily on cervical cancer prevention, public health efforts have neglected the broader implications of HPV on male reproductive health. As researchers continue to uncover the hidden effects of HPV on male fertility, it is increasingly clear that a more inclusive approach to vaccination and prevention is needed to combat this common infection.
The impact of HPV on male fertility is a critical issue that demands greater attention and action. The findings from Argentina highlight the need for comprehensive vaccination programs that prioritize the health of both males and females. By rethinking HPV as a gender-neutral health concern, we can work towards eradicating this virus and protecting the reproductive health of future generations.

Leave a Reply